Antibiotic Resistance: Challenges and Consequences
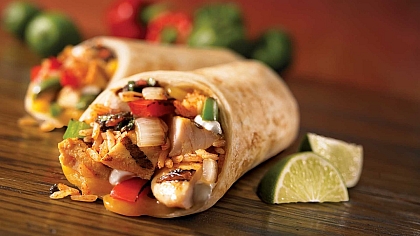
Antibiotics and their resistance have a surprising connection to the world of food. In agriculture, antibiotics are often used to promote growth and prevent disease in livestock, a practice that has contributed to the rise of antibiotic-resistant bacteria. These resistant strains can find their way into the food chain, impacting public health and the safety of what we eat.
Addressing antibiotic resistance involves rethinking agricultural practices, supporting sustainable farming methods, and making informed food choices to protect both human health and the environment. This highlights the critical link between what we consume and the global fight against antibiotic resistance.
Antibiotics have been a cornerstone of modern medicine, revolutionizing the treatment of bacterial infections and saving countless lives. However, the overuse and misuse of these life-saving drugs have given rise to a significant global health challenge: antibiotic resistance.
We will explore the history of antibiotics, the emergence of antibiotic resistance, its consequences, and the ongoing efforts to address this critical issue.
A Brief History of Antibiotics
Antibiotics, such as penicillin, were first discovered in the early 20th century and marked a turning point in treating bacterial infections. They allowed medical professionals to combat illnesses from minor skin infections to life-threatening diseases like pneumonia and sepsis. However, as antibiotics became more widely available, their misuse and overuse started to fuel the development of antibiotic resistance.
The Emergence of Antibiotic Resistance
Antibiotic resistance occurs when bacteria evolve mechanisms to withstand the effects of antibiotics. This can happen when bacteria are exposed to antibiotics, and those with natural resistance survive and reproduce, passing their resistance to the next generation. Over time, this can lead to the development of antibiotic-resistant strains, making infections more challenging to treat.
Consequences of Antibiotic Resistance
- Increased Mortality: Antibiotic-resistant infections are often more challenging to treat, leading to higher mortality rates. Common infections like pneumonia and urinary tract infections become life-threatening when antibiotics are ineffective.
- Prolonged Illness: Patients with antibiotic-resistant infections may face longer and more complicated treatment courses, resulting in extended suffering and healthcare costs.
- Impact on Healthcare Systems: The rise of antibiotic-resistant infections significantly burdens healthcare systems. Hospitals must implement stringent infection control measures, and the cost of care for resistant diseases is substantially higher.
- Global Health Threat: Antibiotic resistance knows no borders. Resistant bacteria can spread globally, making it a challenge that requires international cooperation to address effectively.
Contributing Factors to Antibiotic Resistance
Several factors have contributed to the development of antibiotic resistance, including:
- Overprescribing: Inappropriate or unnecessary prescription of antibiotics for viral infections, which antibiotics cannot treat, has contributed to resistance.
- Incomplete Courses: Patients not finishing a prescribed course of antibiotics can leave behind the most resistant bacteria, allowing them to thrive.
- Misuse in Agriculture: Using antibiotics in animal agriculture for growth promotion has contributed to the spread of resistance.
Addressing Antibiotic Resistance
- Responsible Prescribing: Healthcare providers play a crucial role in responsible antibiotic use, ensuring that antibiotics are only prescribed when necessary.
- Patient Education: Raising awareness among patients about the importance of taking antibiotics as prescribed and the consequences of misuse.
- Research and Development: Scientists are actively researching and developing new antibiotics and alternative treatments to combat resistant bacteria.
- Global Cooperation: International efforts to address antibiotic resistance include surveillance, data sharing, and the development of common strategies.
Antibiotics have been instrumental in modern medicine, saving lives and transforming healthcare. However, the emergence of antibiotic resistance poses a significant threat to global health. The history of antibiotics highlights their life-saving potential, while the challenges of resistance underscore the need for responsible antibiotic use, patient education, and ongoing research and development.
Combating antibiotic resistance is essential to ensure these crucial drugs effectively treat bacterial infections. The fight against antibiotic resistance is a shared responsibility that requires collaboration among healthcare providers, researchers, policymakers, and the public to preserve the efficacy of antibiotics for generations to come.